Did you know that the Affordable Care Act (ACA) has facilitated over 20 million previously uninsured Americans in acquiring health coverage? Enacted in March 2010, this healthcare reform law, commonly referred to as Obamacare, aimed to extend health insurance to millions of uninsured individuals and transform the broader healthcare landscape in the United States. But what is the ACA, and how does it affect you?
The ACA introduces several critical changes. It expands Medicaid, establishes health insurance exchanges, and most significantly, bans insurance companies from denying coverage due to pre-existing conditions. These reforms collectively aim to enhance healthcare accessibility, affordability, and efficiency. Whether you are an individual seeking coverage or an employer facing new responsibilities, grasping the ACA’s provisions is essential for making informed health decisions.
Key Takeaways
- The Affordable Care Act (ACA) has provided health insurance to over 20 million previously uninsured Americans.
- Key reforms include expanding Medicaid and establishing health insurance exchanges.
- The ACA prohibits insurance companies from denying coverage due to pre-existing conditions.
- The law emphasizes preventive care and aims to reduce healthcare costs.
- Understanding the ACA is critical for both individuals and employers navigating the healthcare system.
Understanding the Affordable Care Act (ACA)
The Affordable Care Act (ACA), a landmark health reform law enacted in 2010, aims to provide affordable health insurance to more Americans and improve the quality of care. The fundamental ACA definition and principles revolve around reducing healthcare costs, expanding healthcare coverage, and improving the efficiency of the U.S. healthcare system.
One of the core components under ACA guidelines is the individual mandate, which stipulates that all citizens must have health insurance or pay a penalty. This provision is designed to ensure that everyone contributes to the health insurance pool, lowering overall costs. Employer mandates are also enforced, requiring businesses with 50 or more full-time employees to offer health insurance that meets specific coverage standards.
Another critical aspect of the ACA involves the establishment of health insurance exchanges. These platforms allow individuals and small businesses to compare different health insurance plans and purchase coverage that fits their needs. By providing a competitive marketplace, these exchanges strive to make healthcare more accessible and transparent.
Essential benefits under the ACA requirements include a variety of services designed to cover all health needs:
- Outpatient care
- Emergency services
- Hospitalization
- Maternity and newborn care
- Mental health services
- Prescription drugs
- Rehabilitative services
- Laboratory services
- Preventive and wellness services
- Pediatric services
These mandated benefits ensure that every insurance plan under the ACA provides a baseline level of coverage. This safeguards the health and financial well-being of Americans. Understanding these key elements helps in grasping the broader ACA definition and its practical implications on the health landscape.
| Component | Description |
|---|---|
| Individual Mandate | Requires citizens to have health insurance or face penalties. |
| Employer Mandate | Requires employers with 50+ full-time employees to offer health insurance. |
| Health Insurance Exchanges | Marketplaces for comparing and purchasing insurance plans. |
| Essential Benefits | Includes outpatient care, emergency services, and more. |
By comprehending these elements of ACA guidelines, individuals and businesses can better navigate the health insurance landscape. They can ensure compliance with ACA requirements.
The History of the ACA
The ACA history is a seminal chapter in the evolution of healthcare reform within the United States. Initiated by President Barack Obama, the ACA sought to rectify the disparity in healthcare access for millions of Americans. The legislative journey of the Affordable Care Act commenced with its introduction in the House of Representatives in 2009. By March 2010, the Act was ratified, amidst a backdrop of intense political polarization.
The introduction of health insurance exchanges in 2014 was a critical juncture in the ACA’s legislative timeline. These exchanges facilitated the creation of marketplaces where individuals could engage in the comparison and acquisition of insurance plans, broadening the spectrum of available coverage.
Concurrently, the ACA’s expansion of Medicaid eligibility was a cornerstone of the Obama administration’s healthcare reforms. This expansion targeted lower-income individuals who had hitherto been excluded from healthcare access, embodying the administration’s commitment to inclusivity and accessibility.
The ACA’s history is characterized by unwavering efforts to navigate through numerous challenges and obstacles. Despite formidable opposition, the Obama administration’s healthcare agenda achieved significant progress toward a more equitable healthcare system. The implementation of key provisions was staggered over several years, allowing for continuous refinement and enhancement.
The table below delineates some of the most significant milestones in the ACA’s legislative timeline, underscoring the profound impact of Obama’s healthcare reforms:
| Year | Milestone |
|---|---|
| 2009 | Introduction of the Affordable Care Act in the House of Representatives |
| 2010 | Signing of the ACA into law |
| 2014 | Launch of Health Insurance Exchanges |
| 2014 | Expansion of Medicaid eligibility |
How the ACA Changed Health Insurance
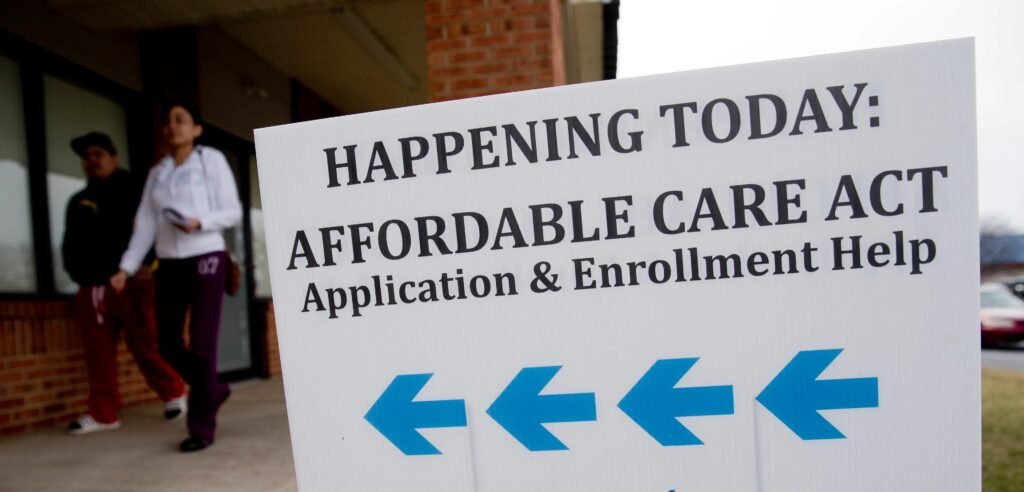
The Affordable Care Act (ACA) has profoundly reshaped the U.S. health insurance sector. A cornerstone of these changes is the mandate for insurance coverage, ensuring universal access to health insurance. This legislative innovation aimed to rectify the issue of uninsured Americans, catalyzing a significant healthcare expansion.
The ACA also introduced health insurance exchanges to foster competitive pricing. These online platforms empower individuals and families to compare and acquire health insurance plans, fostering a more transparent and consumer-centric environment. A vital aspect of this expansion is the inclusion of essential health benefits, which mandates insurers to offer standardized, all-encompassing coverage.
The Medicaid expansion further bolstered coverage, extending eligibility to those with incomes up to 138% of the federal poverty level. Simultaneously, subsidies were introduced for those purchasing private insurance, making it more accessible to individuals and families up to 400% of the federal poverty level. This integrated strategy has been instrumental in diminishing the uninsured and underinsured populations, ensuring wider healthcare access and the provision of essential health benefits.
Key Terms to Know
Grasping the Affordable Care Act (ACA) necessitates comprehension of several critical elements. The individual mandate, a cornerstone of the ACA, mandates that all Americans secure health insurance. This stipulation necessitates individuals to acquire health insurance or incur a penalty. It aims to foster a balanced demographic within the insurance market, ensuring stability through a mix of healthy and sick individuals.
The concept of health insurance subsidies is equally vital. These subsidies, commonly known as advanced premium tax credits, are dispensed on a sliding scale basis, contingent upon income. Their purpose is to render insurance more accessible to lower and middle-income households and families who procure coverage through the ACA exchanges. This endeavor by the ACA extends healthcare accessibility to a wider demographic, concurrently alleviating the financial strain associated with health insurance premiums.
To further elucidate these ACA key terms:
- Individual Mandate: A requirement for all Americans to have health insurance, with penalties applied for non-compliance, ensuring a diverse mix of insured individuals.
- Health Insurance Subsidies: Financial assistance provided to eligible individuals and families, calculated based on income, to help cover the costs of premiums for plans purchased through the ACA exchanges.
Comprehension of these ACA key terms is imperative for navigating the intricacies of the health insurance domain. It facilitates informed decision-making regarding coverage and financial planning.
Enrollment in ACA Plans
ACA enrollment is a critical process, enabling individuals and families to acquire health insurance. The primary avenue for enrolling in ACA plans is through the annual open enrollment period, spanning from November 1 to December 15. This timeframe allows for the selection, renewal, or modification of health insurance plans.
Outside the confines of the open enrollment period, individuals can pursue coverage through special enrollment periods (SEPs). SEPs are accessible post-certain life events, such as marriage, childbirth, or the loss of other health coverage. These special enrollment periods are designed to ensure uninterrupted coverage during critical life transitions.
| Enrollment Type | Period | Eligibility Criteria |
|---|---|---|
| Open Enrollment | November 1 – December 15 | Any individual seeking ACA coverage |
| Special Enrollment Period | Varies based on qualifying event | Eligible individuals experiencing life events such as marriage, childbirth, or loss of coverage |
“Open enrollment periods provide a critical window for individuals to select and update their health insurance plans, ensuring coverage for the upcoming year. Simultaneously, special enrollment periods offer flexibility for life changes, facilitating stable coverage during transitional phases.” – [HealthCare.gov]
The Impact on Consumers

The Affordable Care Act (ACA) has profoundly reshaped the healthcare landscape, introducing both advantages and obstacles for consumers. A significant ACA consumer impact is the expansion of insurance coverage, which has diminished the uninsured populace. The Centers for Disease Control and Prevention (CDC) reports a decline in the uninsured rate from 16% in 2010 to 8.9% in 2021, underscoring the ACA’s success in broadening healthcare access.
The financial implications, though, present a more nuanced scenario. While subsidies have rendered insurance more accessible for many, others have encountered hikes in ACA costs, most prominently in premiums. This disparity has ignited discussions regarding the ACA’s cost management and efficiency.
Further, deductibles and out-of-pocket expenses have escalated for some, creating hurdles despite the enhanced healthcare access. These increasing expenditures underscore that, while more individuals are insured, the affordability of healthcare services remains a pressing concern for a portion of the populace.
Conversely, the ACA has facilitated a greater number of people accessing preventive services and treatments, contributing to enhanced public health outcomes. The uptick in preventive care access highlights the ACA’s role in averting long-term health problems, ultimately benefiting the broader society. Yet, the ongoing challenge lies in balancing the enhancement of healthcare access with the management of escalating ACA costs.
Employer Responsibilities Under the ACA
The Affordable Care Act (ACA) mandates critical responsibilities for employers, predominantly through the ACA employer mandate. This mandate necessitates businesses with 50 or more full-time employees to offer health insurance coverage. Non-compliance could incur substantial penalties, underscoring the imperative of understanding and adhering to the mandate.
Compliance with the ACA transcends mere provision of insurance. Employers must also fulfill specific reporting obligations. They are required to submit detailed information to the IRS regarding the health coverage offered and its associated costs. This transparency is instrumental in ensuring adherence to ACA standards.
An examination of the ACA employer mandate reveals a multitude of employer responsibilities. Employers must meticulously manage their employee benefits strategies to comply. The ACA’s demands have fundamentally reshaped how businesses approach health insurance, highlighting the critical need for accurate, up-to-date knowledge of compliance regulations.
Maintaining ACA compliance is not only vital for avoiding penalties but also for advancing the ACA’s broader goal of expanding health insurance coverage through workplace benefits. Effective compliance strategies enhance employee health and well-being, reinforcing the ACA’s foundational objectives.
In conclusion, the ACA employer mandate encompasses a detailed set of employer responsibilities. Employers must provide adequate health coverage and ensure thorough reporting to fulfill their ACA obligations. This contributes to the overarching mission of accessible healthcare for all.
Challenges and Controversies
From its inception, the Affordable Care Act (ACA) has faced numerous ACA challenges, often catalyzed by political opposition from lawmakers who contest its provisions. These challenges have manifested in multiple attempts to repeal or significantly alter key elements of the act. Critics contend that the costs of implementing the ACA outweigh its benefits, whereas proponents highlight the increased healthcare access it has facilitated.
The public perception of ACA remains polarized. Some commend the law for expanding coverage to millions of uninsured Americans and reducing healthcare disparities. In contrast, others decry the mandate provisions and the economic repercussions for businesses and individuals. This dichotomy perpetuates the ongoing debate regarding the ACA’s efficacy and future.
Misconceptions about the ACA’s detailed provisions significantly contribute to its controversy. For instance, some individuals believe the ACA imposes excessive financial burdens, while others perceive it as insufficient in ensuring affordable healthcare for all. These divergent perspectives underscore the persistent debates and underscore the necessity for clearer communication and comprehension of the law’s actual impacts and intentions.
To better comprehend these challenges, it is essential to examine the viewpoints of various stakeholders:
| Stakeholder | Perspective | Common Challenges |
|---|---|---|
| Lawmakers | Divided between support and opposition | Legislative efforts to repeal or modify the ACA |
| Healthcare Providers | Supportive but concerned about reimbursement rates | Administrative burdens and efficiency constraints |
| Business Owners | Concerned with cost and mandate compliance | Financial and operational impacts |
| General Public | Mixed, depending on access and costs | Understanding of benefits, affordability |
The complexities of the ACA challenges, exacerbated by diverse levels of political opposition and the nuanced public perception of ACA, indicate that the discourse surrounding this landmark legislation is far from resolved. To foster a constructive dialogue, it is imperative to address these misconceptions and consider both the ACA’s positive impacts and criticisms.
Future of the Affordable Care Act
The trajectory of the Affordable Care Act (ACA) is subject to the vicissitudes of political landscapes and the ebb and flow of legislative and judicial deliberations. The influence of successive administrations on ACA’s framework is profound, capable of either fortifying its core or precipitating its erosion. The ACA’s inherent adaptability allows for enhancements that could elevate its efficacy in addressing the healthcare exigencies of the populace. Concurrently, it harbors the risk of modifications that could compromise its fundamental objectives.
Legal disputes surrounding the ACA persist, with the individual mandate, a cornerstone of the act, being a focal point of contention. The Supreme Court’s ruling on the penalty’s invalidation has catalyzed a renewed discourse on the ACA’s sustainability and enforceability. The ACA’s implementation across states reveals a patchwork of policies, with some embracing Medicaid expansion and others eschewing it. This variability in state-level responses to the ACA contributes to disparities in access and effectiveness, influencing the act’s overall reputation and efficacy.
As we traverse the landscape of ACA policy revisions, it is evident that healthcare reform remains a linchpin in American politics and personal lives. The ACA’s capacity to evolve in response to the healthcare sector’s transformations and fulfill the healthcare needs of all citizens hinges on forthcoming adjustments and interpretations. A nuanced comprehension of these dynamics is imperative for those seeking to anticipate the ACA’s future trajectory.